Each week, Chronicle reporters field questions about COVID-19, safety precautions and vaccines. In this week’s COVID Help Desk, we tackle smell recovery for longhaul COVID patients, breakthrough infections, whether the vaccine is lowering the number of severe COVID cases and hospitalizations and the Lambda variant.
For many people who contracted the virus, a loss or change of smell was one of their first symptoms.
Dr. Tran Locke, assistant professor of otolaryngology at Baylor College of Medicine, said there’s no clear answer yet as to whether all COVID survivors or longhaulers will regain their sense of smell.
Locke sees at least two patients a week who have had smell loss as a result of COVID-19. Some patients have had their smell return completely; others say they often smell something rancid. A subset of her patients can recognize smells, like vanilla, but it’s not quite like it was before.
With other patients who experience smell loss, either from brain injuries or non-COVID viral infection, Locke said what they can smell at one year post-infection is typically their new normal.
COVID survivors can also experience parosmia, a distortion of smell when in presence of that odor, Locke said. “Some people say oranges or coffee can smell or taste like rotten meat or dirty socks,” she said. “This can last for months, and the thought process is that the smell nerve is recovering and can sometimes get rewired, making the wrong connection in the brain which distorts the smell.”
However, patients who report rancid smells have had better outcomes with spontaneous smell recovery, Locke said.
Some Houston COVID survivors have begun smell training, which incorporates essential oils like lemon, eucalyptus, clove and rose into their every day smell routine, she said. Through smell therapy, more than 90 percent of patients who experienced smell loss for non-COVID reasons regained that sense after six months — though it may have been different than it was before, she said.
“People take smell and taste for granted until it’s gone,” Locke said. “From a safety standpoint, not being able to smell is dangerous and longterm loss can lead to depression. It seems minor but it makes a big impact.”
What is a breakthrough infection?
Breakthrough infections happen when a person contracts a virus or disease two weeks or longer after full immunization, said Katelyn Jetelina, an epidemiologist with UTHealth School of Public Health in Dallas.
“It can happen with any vaccine,” Jetelina said. “Our vaccines’ efficacy is amazingly high, but they’re not 100 percent. We expect breakthroughs to happen unfortunately.”
The Centers for Disease Control and Prevention reported more than 157 million Americans have been fully vaccinated as of July 6. In Texas, 12.3 million are fully vaccinated.
Asymptomatic infections among vaccinated people will occur, and there’s evidence that vaccination may make illnesses less severe for those who do have symptoms, the CDC reported. Between Jan. 1 and April 30, the CDC reported that out of 3,880 breakthrough infections, 2,725 people were asymptomatic, 995 were known to be hospitalized (but it’s unclear if it was for COVID or another medical issue), and 160 people died.
Vaccines protect most people from severe cases that lead to hospitalization or death, Jetelina said.
The less efficacious the vaccine, though, the more likely the person could have a breakthrough infection, she added, which explains why people who have received a vaccine in a different country with a lower efficacy rate could be more vulnerable to a breakthrough COVID infection. But that doesn’t mean it will automatically be a severe infection.
“By far, the best protection you can have is the vaccine,” Jetelina said. “There is a small risk if you come in contact with someone who is unvaccinated who is carrying the disease that you may get it. It’s a small risk, but the risk is still there.”
It doesn’t hurt to layer protection, such as a face mask, especially when indoors or in close quarters with people who are not in your household, she added.
Since vaccines are widely available, how severe are positive COVID cases that lead to hospitalization?
COVID hospitalizations at two Houston hospitals have doubled in the last two weeks, and health officials are attributing it to a rise in Delta variant cases.
Houston Methodist sequences for specific variants, and models estimate the Delta variant will make up 92 percent of all new infections in the coming weeks. More than 40 percent of new COVID hospitalizations since mid-June are Delta cases, according to spokesperson Lisa Merkl.
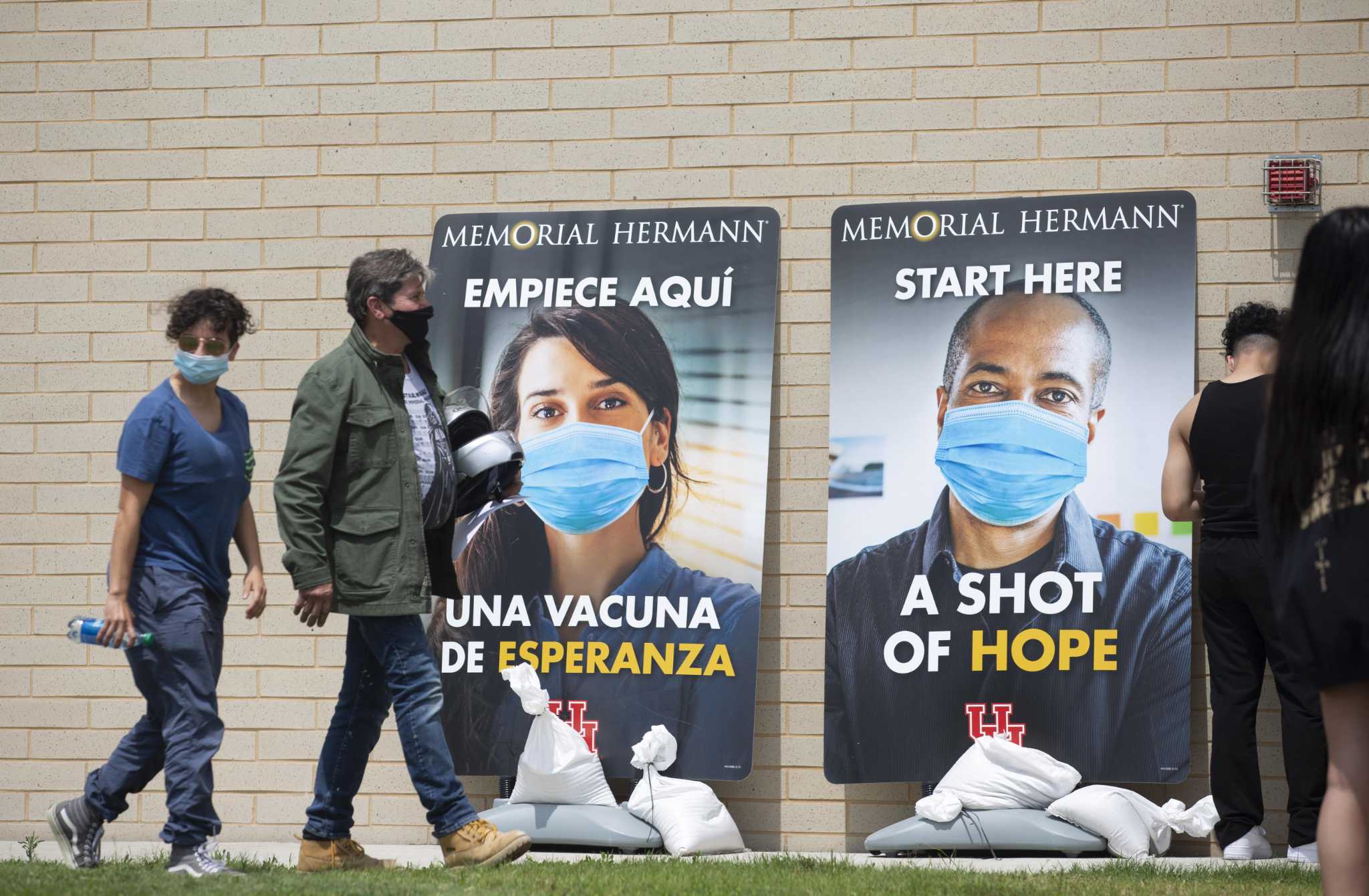
Dr. David Callender, president and CEO of Memorial Hermann, said the system is seeing the effect of the fast-moving variant because of a drastic increase in positive cases coming into the emergency departments. But he said they don’t test for specific variants because treatment is the same.
Out of 55 positive cases identified Monday in Memorial Hermann’s emergency rooms, 35 were sent home to isolate and 20 were admitted to the hospital because their symptoms were severe enough to warrant it, Callender said.
Callender said the vaccines are “certainly holding,” which means few of the new hospitalized patients are vaccinated. “By and large, the people we’re seeing are not vaccinated,” he said.
Should we be concerned about the lambda variant?
The CDC routinely monitors viral mutations and variants through sequencing positive COVID-19 tests and then classifies them as a variant of interest, variant of concern and variant of high consequence.
Variants of interest are more transmissible than the original strain, have caused outbreaks in multiple countries, and could cause more severe illness, but have limited prevalence in the U.S. or other countries, according to the World Health Organization.
Variants of concern show evidence of increased transmissibility, more severe disease, significant reduction in neutralization by antibodies generated during previous infection or vaccination and reduced effectiveness of treatments or vaccines. As of Tuesday, U.S. variants of concern were listed as B.1.1.7 (alpha), B.1.351 (beta), B.1.617.2 (delta) and P.1 (gamma).
C.37, or the lambda variant, is listed as a variant of interest in the U.S., although it’s spreading quickly in South America. The earliest cases were found in Peru in December, and now lambda accounts for 90 percent of Peruvian infections, according to the country’s health ministry.
Researchers will continue to monitor the spread of lambda because of a specific mutation in its spike protein that may increase the virus’ infectiousness, said Dr. Pei-Yong Shi, professor of biochemistry and molecular biology at UTMB.
The mutated virus shows little improvement when treated with monoclonal antibodies through convalescent plasma therapy, Shi said.
“Once you have that mutation, it confers resistance to several monoclonal antibodies, including those approved by the FDA to treat coronavirus symptoms,” Shi said. “It’s something that needs to be closely monitored, but I’m not aware of it being more transmissible (than the original virus).”
CDC data suggests vaccines authorized for use in the U.S. — Pfizer, Moderna and Johnson & Johnson — protect against most variants currently circulating in the country. The strain has been located in 29 countries states so far, according to National Geographic.
“However, variants will cause some vaccine breakthrough cases,” the CDC reported.
julie.garcia@chron.com
Twitter.com/reporterjulie
"smell" - Google News
July 16, 2021 at 06:07PM
https://ift.tt/3kqO0IW
COVID Help Desk: I recovered from the virus. Will my sense of taste and smell ever return? - Houston Chronicle
"smell" - Google News
https://ift.tt/35zrwu1
https://ift.tt/3b8aPsv
Bagikan Berita Ini


















0 Response to "COVID Help Desk: I recovered from the virus. Will my sense of taste and smell ever return? - Houston Chronicle"
Post a Comment